Disclaimer: Individual results vary, not all patients respond. Additional doses may be necessary to maintain the clinical response. Treatment for these indications is innovative (“off-label”). Please see the Terms of Use. The method of off-label treatment utilized is a patented invention of TransBarrier®.
Author: Webmaster
Rapid improvement in hand function after treatment at TransBarrier® 5 years after stroke, September 2016
Patient from Georgia has rapid improvement in hand function after treatment at TransBarrier®, September 2016, 5 years after stroke!
Disclaimer: Individual results vary, not all patients respond. Additional doses may be necessary to maintain the clinical response. Treatment for these indications is innovative (“off-label”). Please see the Terms of Use. The method of off-label treatment utilized is a patented invention of TransBarrier®.
Able to Run Minutes After Treatment at TransBarrier® 2 Years after Stroke, September 2016
Patient from Oklahoma is able to run minutes after treatment by TransBarrier® two years after stroke!
Disclaimer: Individual results vary, not all patients respond. Additional doses may be necessary to maintain the clinical response. Treatment for these indications is innovative (“off-label”). Please see the Terms of Use. The method of off-label treatment utilized is a patented invention of TransBarrier®.
Sunday Night (TV) News Story in Australia
“The New Stroke Treatment That’s Changing Lives”
Sunday Night (Australia), March 29, 2015
On March 29, 2015 the television news program “Sunday Night” in Australia aired a national news feature story about TransBarrier® stroke treatment. The story was entitled “The New Stroke Treatment That’s Changing Lives”, and it is accessible online at this link:
Sunday Night “The New Stroke Treatment That’s Changing Lives”.
In the television feature, the clinical results of two patients treated at TransBarrier® Los Angeles are depicted. The story was filmed both in Los Angeles at the time of treatment and in Australia, after each of the patients returned home.
Disclaimer: Individual results vary, not all patients respond. Continuing maintenance treatment may be necessary to maintain the clinical response. Treatment for this indication is off-label. Please see the Terms of Use. The method of treatment utilized is a patented invention of TransBarrier®. Issued and pending U.S. and foreign patents, including, but not limited to, U.S. 6419944, 6537549, 6982089, 7214658, 7629311, 8119127, 8236306, 8349323 and 8900583 all assigned to TACT IP, LLC; and Australian patent 758523.
Randomized, double-blind, placebo-controlled anti-TNF for AD clinical trial results publish
Issue 10, volume 4, Supplement of Alz and Dementia: Journal of the Alz Association, Session 04-11-02, P273, entitled “The Safety and Tolerability of [TNF Inhibitor] in AD (STEADI-09): A Phase II Double Blind Randomised Placebo Controlled Trial”, principal investigator Clive Holmes MD, University of Southampton, Southampton, United Kingdom, contains the first double-blind, randomized, placebo-controlled data supporting the therapeutic efficacy of anti-TNF for treatment of AD. The abstract of this study (full-text here) published in this issue in July 2014.
A 2008 article in BBC News had previously discussed the favorable results of anti-TNF for treatment of AD in a study from TransBarrier® The article reported at the time that Clive Holmes MD was interested in taking on further research utilizing this treatment approach.
Further recognition of the scientific rationale for TNF inhibition in stroke models
May 10, 2014
Two scientists from the UCLA Department of Neurology have published a new research article entitled “Intracerebral hemorrhage in mouse models: therapeutic interventions and functional recovery“, Metab Brain Dis. 2014 epub May 10.
The authors recognize intracerebral hemorrhage as a subtype of focal stroke and the most common form of brain hemorrhage. The authors explain,
“With direct blood extravasation into brain, secondary inflammation is a substantial feature. Drugs which reduce neuroinflammation enhance functional recovery. Lei and colleagues targeted tumor necrosis factor alpha (TNF-alpha), a cytokine that is secreted by the microglia in response to injury and acts as a prime neuroinflammatory mediator causing progressive damage. A single dose of TNF-alpha antibody … showed evidence of reduced neuroinflammation and improved functional deficit….”
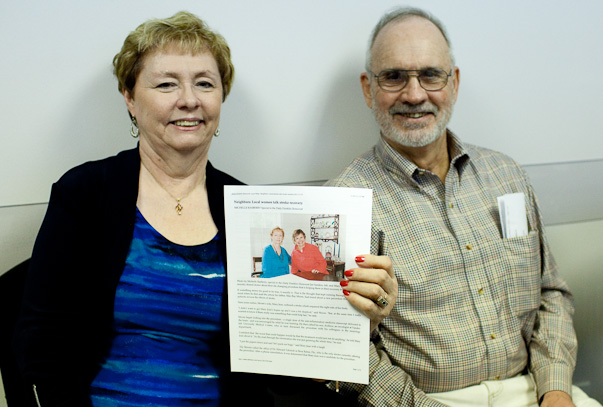
Jan Sanders returns to Boca Raton from Kennett, Missouri on March 11, 2013
We were pleased that Jan returned to visit us on March 11 from Kennett, Missouri with her husband. She is holding the story the Daily Dunklin Democrat had printed on February 17 about her rapid clinical improvement after treatment. To read the whole story please visit the story on the webpage of the Daily Dunklin Democrat (click here).
Basic Science News: TNF inhibition reduces neurovascular injury after Intracerebral Hemorrhage
TNF-alpha receptor antagonist, R-7050, improves neurological outcomes following intracerebral hemorrhage in mice
Melanie D. King,
Cargill H. Alleyne Jr.,
Krishnan M. Dhandapani
Department of Neurosurgery, Medical College of Georgia, Georgia Regents University, Augusta, GA, USA
Abstract
Intracerebral hemorrhage (ICH), the most common form of hemorrhagic stroke, exhibits the highest acute mortality and the worst long-term prognosis of all stroke subtypes. Unfortunately, treatment options for ICH are lacking due in part to a lack of feasible therapeutic targets. Inflammatory activation is associated with neurological deficits in pre-clinical ICH models and with patient deterioration after clinical ICH. In the present study, we tested the hypothesis that R-7050, a novel cell permeable triazoloquinoxaline inhibitor of the tumor necrosis factor receptor (TNFR) complex, attenuates neurovascular injury after ICH in mice. Up to 2 h post-injury administration of R-7050 significantly reduced blood–brain barrier opening and attenuated edema development at 24 h post-ICH. Neurological outcomes were also improved over the first 3 days after injury. In contrast, R-7050 did not reduce hematoma volume, suggesting the beneficial effects of TNFR inhibition were downstream of clot formation/resolution. These data suggest a potential clinical utility for TNFR antagonists as an adjunct therapy to reduce neurological injury and improve patient outcomes after ICH.
Jan Sanders and Mary Jean Moore discuss their treatment results in the Daily Dunklin Democrat
http://www.recorder.com/home/
Science News: New pathology study: Inflammation persists for years after a single traumatic brain injury
Brain. 2013 Jan;136(Pt 1):28-42. doi: 10.1093/brain/aws322.
Inflammation and white matter degeneration persist for years after a single traumatic brain injury.
Johnson VE, Stewart JE, Begbie FD, Trojanowski JQ, Smith DH, Stewart W.
Source
Penn Centre for Brain Injury and Repair and Department of Neurosurgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104, USA.
Abstract
A single traumatic brain injury is associated with an increased risk of dementia and, in a proportion of patients surviving a year or more from injury, the development of hallmark Alzheimer’s disease-like pathologies. However, the pathological processes linking traumatic brain injury and neurodegenerative disease remain poorly understood. Growing evidence supports a role for neuroinflammation in the development of Alzheimer’s disease. In contrast, little is known about the neuroinflammatory response to brain injury and, in particular, its temporal dynamics and any potential role in neurodegeneration. Cases of traumatic brain injury with survivals ranging from 10 h to 47 years post injury (n = 52) and age-matched, uninjured control subjects (n = 44) were selected from the Glasgow Traumatic Brain Injury archive. From these, sections of the corpus callosum and adjacent parasaggital cortex were examined for microglial density and morphology, and for indices of white matter pathology and integrity. With survival of ?3 months from injury, cases withtraumatic brain injury frequently displayed extensive, densely packed, reactive microglia (CR3/43- and/or CD68-immunoreactive), a pathology not seen in control subjects or acutely injured cases. Of particular note, these reactive microglia were present in 28% of cases with survival of >1 year and up to 18 years post-trauma. In cases displaying this inflammatory pathology, evidence of ongoing white matter degradation could also be observed. Moreover, there was a 25% reduction in the corpus callosum thickness with survival >1 year post-injury. These data present striking evidence of persistent inflammation and ongoing white matter degeneration for many years after just a single traumatic brain injury in humans. Future studies to determine whether inflammation occurs in response to or, conversely, promotes white matter degeneration will be important. These findings may provide parallels for studying neurodegenerative disease, withtraumatic brain injury patients serving as a model for longitudinal investigations, in particular with a view to identifying potential therapeutic interventions.